Featured Items

A New Coronavirus, a New Epidemic, Many Open Questions

Adelaida Sarukhan*
Latest update: May 07, 2021
The new coronavirus that jumped from some animal to a person in the city of Wuhan at the end of last year has managed, in only a few weeks, to draw huge attention from the media, scientists and the international community. On January 30, the WHO declared the epidemic a public health emergency of international concern (PHEIC).
The epidemic is evolving very fast and with it, the knowledge we have on this new virus. From not knowing anything at beginnings of 2020, the scientific community has managed to isolate it, sequence it, identify it, and develop a diagnostic test.
However, as occurs with every new epidemic, there are many open questions that will be answered as the epidemic evolves and as scientists manage to get a better grasp of the virus’s behaviour.
On this page, we offer relevant information on the virus and the pandemic, through the content below as well as links to more specific content such as analysis and opinion articles, and videos.
COVID-19: Scientific Updates |
Policy Documents | COVID-19 and Response Strategy |
 Support our research against COVID-19. Donate here! |
1. What is the New Coronavirus SARS-CoV-2 or COVID-19?
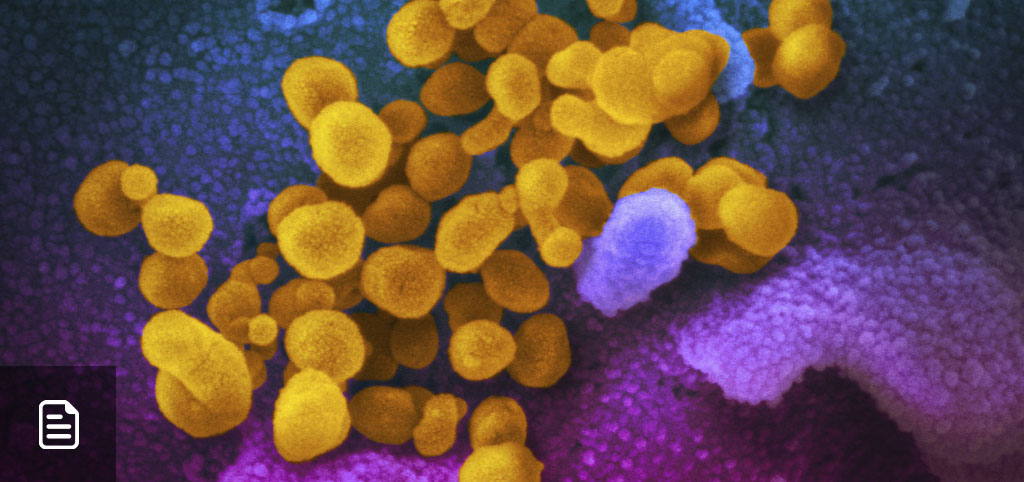
The new coronavirus, first called 2019-nCoV and officially renamed as SARS-CoV2 (the virus) and COVID-19 (the disease), belongs to the family of coronavirus, which owe the name to crown-like spikes on their surface. Most described coronavirus are found in birds or mammals, particularly bats.
The new coronavirus is called SARS-CoV2 because its genetic sequence is very similar to that of SARS, another coronavirus that appeared for first (and only) time in 2002 and caused a pandemic with more than 8,000 infected people and 800 deaths. Another coronavirus that causes severe disease in humans is MERS-CoV, identified for the first time in 2012 in the Middle East and associated with camels.
2. How Did SARS-CoV2 Appear?
The SARS-CoV-2 virus is very similar to other coronaviruses found in bats. Although exactly how, when and where the new coronavirus emerged remains unknown, the most likely scenario is that it jumped from a bat to an intermediary mammal host (maybe the pangolin) and from there to humans. The first reported outbreak of cases is associated with a wildlife market in Wuhan. However, a WHO-led mission recently concluded that the market probably served to amplify the outbreak but that there may have been cases before and beyond the market.
3. How Does COVID19 Spread?
The main transmission route of the new coronavirus is by air, through small droplets expelled when someone coughs, sneezes or talks, as well as aerosols (smaller drops capable of travelling further and remain suspended in air) that accumulate in closed and badly ventilated spaces. The virus can also be transmitted by touching your eyes, nose, or mouth after touching contaminated surfaces, although this transmission route seems to be rare.
In contrast with SARS that was only transmitted by people with symptoms, the new coronavirus can be transmitted a day or two before the onset of symptoms (presymptomatic) or even by people who never develop clinical symptoms (asymptomatic). This considerably hinders containment efforts aimed at limiting viral spread and is the reason why everyone should wear a facemask and adhere to social distancing.
COVID-19 can be transmitted from one person to another with considerable ease. To date, the WHO estimates that the R0, or basic reproduction number, the virus is somewhere between 1.4 and 2.5, although other estimates give a range between 2 and 3. This means that every infected person can in turn infect 2 to 3 other people, although “superspreader” people or events play an important role in transmission - it is believed that 20% of cases may account for up to 80% of new infections.
To control an epidemic, the R0 needs to be below 1.
How is COVID-19 diagnosed?
Active infections: look for the virus: SARS-Cov2 infection occurs mainly in the respiratory tract. This is why the diagnostic tests that rely on the amplification of viral gene sequences by PCR must be done on nose or throat swabs. It is important to bear in mind that PCR tests do not distinguish between viable virus and viral fragments. In addition, the result can depend of how the sample is taken.
Other diagnostic tests detect viral proteins (rapid antigen tests) - they are less sensitive (i.e. they do not detect all those infected) but are faster and easier to use, and can identify people who have high viral loads and therefore are highly infectious.
Past infections: Look for antibodies. Another type of test detects virus-specific antibodies. In this case, a blood sample is sufficient. This test detects individuals who have been previously exposed to the virus and could therefore be immune. For the moment, the serological tests used vary widely in terms of sensitivity (capacity to detect positive cases) and specificity (capacity to distinguish from other viruses), so the results must be interpreted with caution. Furthermore, having antibodies to the virus does not guarantee immunity to it. Inversely, cellular immunity (virus-specific T cells) has been observed even in recovered patients with undetectable antibodies.
|
|
4. What are the Symptoms of COVID-19?
The main symptoms are fever, cough and difficulty to breathe. However, in a small percentage of patients, the first symptoms may be headache, nausea or diarrhea. In fact, the virus can also infect other cells of the body, including intestinal cells, which would explain the diarrheas and the presence of viral RNA in stool.
Loss of smell and taste seems to be frequent among infected individuals and could be among the first signs of disease.
An excessive inflammation
SARS-CoV-2 starts replicating in the upper respiratory tract (throat) and in some cases reaches the lungs, where it can cause severe damage (pneumonia and acute respiratory distress). The virus can also infect other cells such as those lining the blood vessels and organs such as the heart, the liver, the kidney and the pancreas. Altogether, this leads to an excessive -and potentially lethal- inflammatory response in patients with advanced disease.
This inflammatory response could also lead to skin rash or red toes observed in some patients. The recent rise in paediatric cases with multisystem inflammatory syndrome (similar to Kawasaki disease) could also be due to an excessive immune response against the coronavirus. However, it is important to point out that these cases are rare.
Incubation Period
The WHO has estimated an incubation period (between infection and symptom onset) of 2 to 14 days, although most people develop symptoms between 5 and 7 days.
How lethal is it?
The fatality rate of the new coronavirus was one of the big unknowns of this pandemic. This is due to the fact that SARS-CoV-2 infection causes a wide range of symptom severity: from lack of symptoms to mild and severe disease, pneumonia, and death. According to an analysis of all 72,342 cases diagnosed in China as of February 11, the disease is mild for 81% of patients, 14% develop severe symptoms, and around 4-5% are critical. More recent data, pooled from 14 European countries, indicate that around 40% of confirmed cases have been hospitalised and 2% of these require critical care.
The great majority of deaths occur in people over 65 years of age and/or with an underlying chronic condition or disease. Major risk factors for severe illness and death include hypertension, diabetes, cardiovascular disease and obesity. Men are more vulnerable to disease then women. In contrast, children are considerably less susceptible to developing the disease, although they do seem to get infected. Their role in spreading the virus remains to be determined.
Initial data suggested a case fatality rate (CFR) of around 2% (which means 2 deaths out of every 100 confirmed cases), but these first estimates did not include asymptomatic or undiagnosed cases. A more recent study estimates that the adjusted case fatality rate in China was 1.4% for confirmed cases and 0.66% when considering infected but undiagnosed cases. Another study based on data from Italy estimates that the lethality rate in Lombardy was of 0.84 for every 100 infected cases.
First results in Spain: The first results of the national seroprevalence study indicate that, between January and beginnings of May, around 5% of the country’s population was infected by the virus. This means that the infection fatality rate in Spain was around 1% (one death for every 100 infected people).
As the pandemic advances, it is clear that the reported fatality rate varies between countries (roughly, between 1 and 10% of confirmed cases), and that this depends on the number of diagnosed individuals and other factors such as the percentage of vulnerable people (elderly or with chronic conditions) and the capacity of health systems.
In any case, the case fatality rate of COVID-19 is lower than that of SARS (10%) and could be up to ten times higher than that of seasonal flu (below 0.1%).
|
|
5. How is COVID-19 Treated?
Treatments
To gain time, the medical community started testing drugs that already existed in the market and that could have an effect on the new virus. Some examples are the antiviral drug remdesivir (originally tested for Ebola virus) and an HIV treatment (lopinavir / ritonavir), as well as chloroquine, an old antimalarial drug. Drugs that can modulate the immune system, such as antibodies against interleukin 6, have been tested with encouraging results. This is because, in patients with severe disease, tissue damage not only results from the virus itself, but from an excess of inflammatory molecules (the so-called cytokine storm).
The repurposed drugs that for the moment have been shown to have an effect in controlled clinical trials are remdesivir (it shortens the number of days spent in intensive care) and steroids (dexamethasone reduces mortality among critically ill patients).
SARS-CoV-2 specific drugs have also been developed. Namely, cocktails of monoclonal antibodies have shown to be effective in limiting disease progression when administered early.
Prevention
The basic preventive measures to avoid infection are: wash your hands frequently, cover your mouth when sneezing or coughing and use a face mask. . It is important to avoid crowds in closed and badly ventilated spaces.
Areas with high viral transmission have adopted stricter social distancing measures, such as cancelling mass gatherings, promoting telework, avoiding unnecessary travel, and keeping a distance of at least 1 meter with other people, among others. These measures, together with the use of face masks, are helping to slow viral spread within the community and avoid overwhelming health systems.
|
|
Vaccines
There are over 150 vaccine candidates in development, of which more than 90 have entered clinical trials in humans. Several have already announced preliminary or final efficacy results and eight have been approved for use in the general population (4 of them in Europe).
6. Evolution of the Epidemic
Key figures
Last update: 07/05/2021 at 3.23 PM. Data from Johns Hopkins University & Medicine.
Source: Our World in Data map with data from Johns Hopkins University.