Comprehensive Models of Care for Non-Alcoholic Fatty Liver Disease (NAFLD)
A group of experts led by the EASL International Liver Foundation and ISGlobal develop a set of eight recommendations to improve care for NAFLD patients
07.07.2021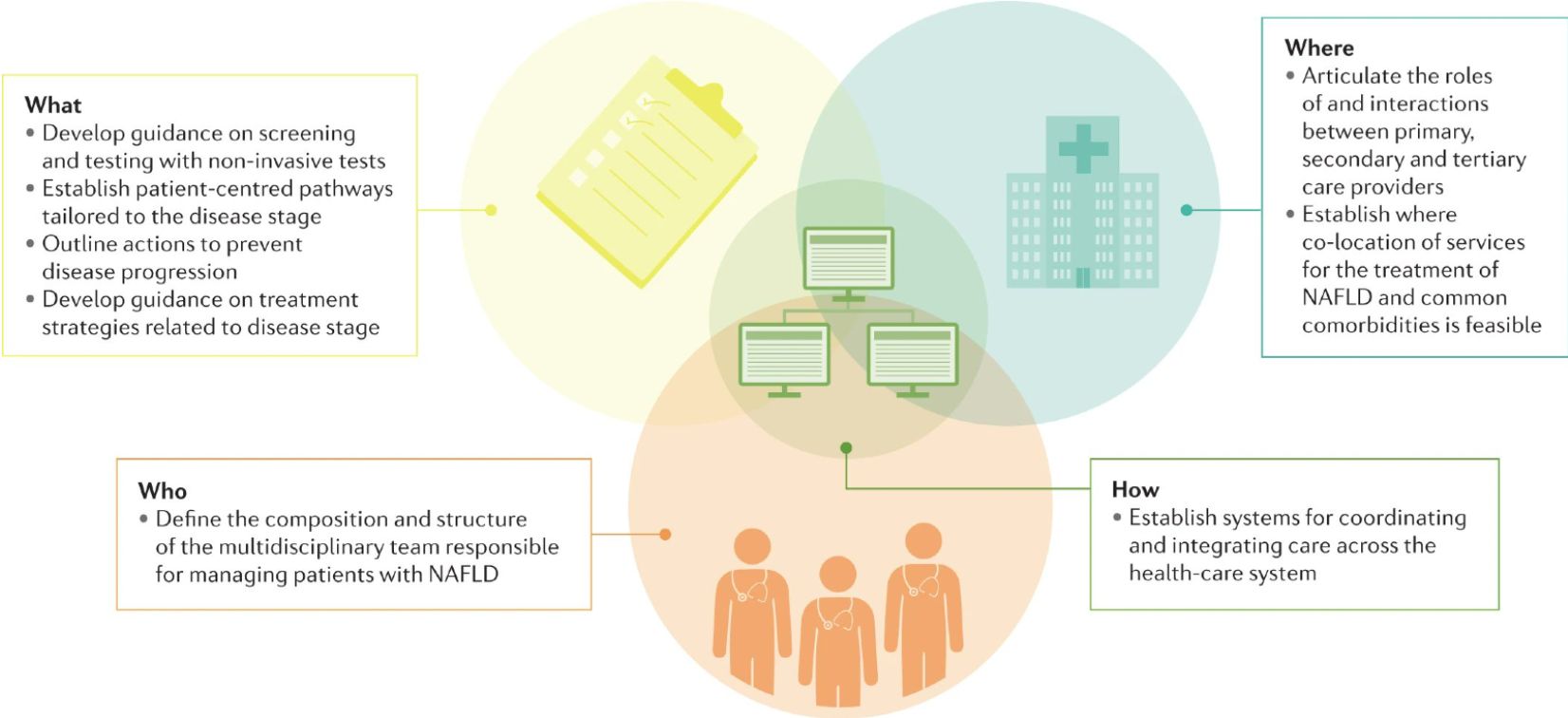
Non-alcoholic fatty liver disease (NAFLD) is the leading cause of chronic liver disease globally. However, despite the increased demand placed on health-care systems, little attention has been given to the management of patients with this disease within health-care settings. Actually, in many health-care settings, no formal pathways exist and, where pathways are in place, they are often not standardized according to good practices.
To help address the increasing need for the provision of good practice care for patients with NAFLD, a group of experts led by the EASL International Liver Foundation (EILF) and the Barcelona Institute for Global Health (ISGlobal) analysed the published review of models of care for NAFLD and developed a set of recommendations for health-care providers and policy-makers seeking to improve these care models and patient outcomes. The conclusions were published in an article in Nature Reviews Gastroenterology & Hepatology during EASL’s International Liver Congress 2021
“The eight recommendations are not intended as a checklist but rather as a framework to help guide practitioners and policy-makers seeking to improve care for people with NAFLD” states Jeffrey V. Lazarus, first author of the article, vice-chair of EILF, and a researcher at ISGlobal. “Indeed, they should be reviewed and updated periodically as we learn more about these care models, including the effect on clinical outcomes and the cost-effectiveness of different approaches.”
The eight recommendations, which detail what services are required by patients, where they should be delivered, who should provide them and how they should be coordinated within health-care systems, are the following:
- Establish clearly defined care pathways tailored to assessing the stage of disease, the presence of comorbidities and the optimal health outcome for the patient.
- Develop guidance on screening and testing with non-invasive tests.
- Develop guidance on treatment strategies for patients, related to their disease stage.
- Outline actions for preventing disease progression in primary care for patients with early-stage disease not requiring specialist hepatology care.
- Articulate and define the roles and interactions between primary, secondary and tertiary care providers.
- Establish where services for NAFLD can be co-located with services for the treatment of common comorbidities.
- Define the composition and structure of the multidisciplinary team responsible for managing patients.
- Establish effective systems for coordinating and integrating care across a health-care system.
Given the increasing prevalence of NAFLD and the low percentage of diagnosed cases, the authors affirm that health systems need to start reorienting to ensure that care can be delivered efficiently and effectively to address this progressive condition and reduce its wide-reaching health implications. These recommendations can contribute to filling the dearth of guidance on NAFLD models of care and help address the increasing need for the provision of best practice care for patients
Reference
Lazarus, J.V., Anstee, Q.M., Hagström, H. et al. Defining comprehensive models of care for NAFLD. Nat Rev Gastroenterol Hepatol (2021). https://doi.org/10.1038/s41575-021-00477-7



