Featured Items

Global Health Lessons From an Epidemic

adelaida sarukhan - ISGlobal's Policy Team*
Last Updated: 17, March 2016
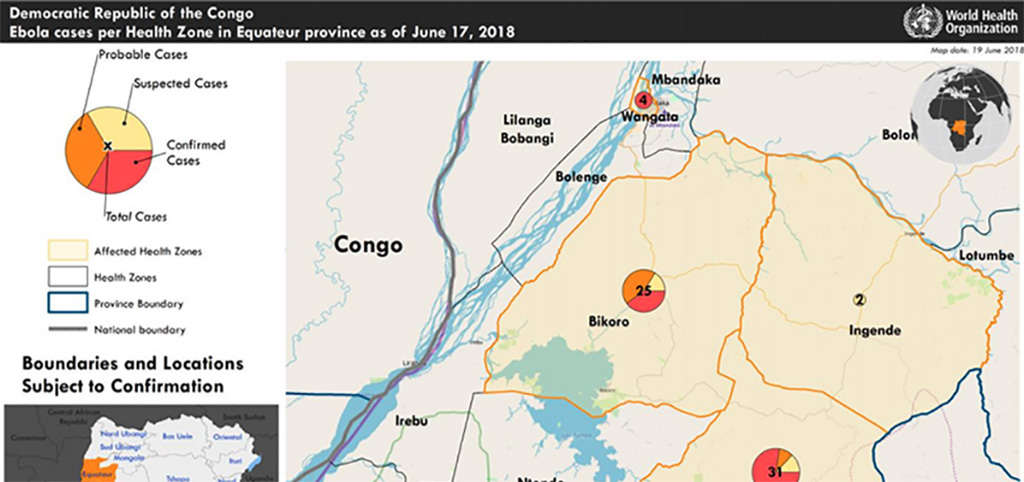
On March 22, two years have passed since the health authorities in Guinea officially declared an outbreak of Ebola in the country. Since then the WHO has declared the region free of Ebola transmission twice, only for new cases to reemerge hours after the announcement. Both occasions have retarded the long-awaited celebration and has highlighted the risk of disease re-emergence due to viral persistance in some survivors.
The most terrifying epidemic of the last years leaves behind a devastating trail that starts with the number of dead (11,300) and infected (28,000) people and that has further weakened the health systems and economic perspectives of a region that was struggling to leave its past behind.
Today we are well aware that the international community’s response was too little and too late. But the grievance of the affected countries and the memory of their victims will be double if, after having allowed the crisis to develop beyond control, we choose to ignore the key lessons that can be drawn. One major lesson is that the fight against Ebola, or any other global health threat, starts well before the first case is diagnosed.
This ISGlobal special offers a general vision of the Ebola crisis and the political, economic and scientific response in the affected and donor countries. With this, we update the information provided one year ago and we provide some thoughts on how this kind of tragedies can be avoided in the future.
What do we know about Ebola?
Ebola is an infectious viral disease that affects humans and nonhuman primates, such as monkeys, gorillas and chimpanzees. Although the virus was identified for the first time in 1976, it has existed for more than 10,000 years. Its natural reservoir is not known with certitude, but the scientific evidence points towards fruit bats. Of the five species of Ebola virus, four can infect humans (Zaire, Sudan, Bundibugyo and Taï) of which the Zaire species is the most lethal of all and has caused the most outbreaks (including the one in West Africa).
Once the virus jumps to humans through contact with bat droppings or consumption of infected bush meat, it is transmitted from human to human by direct contact. Transmission occurs when mucous membranes come in contact with bodily fluids, including sweat, saliva, stool and semen of infected patients or bodies. Despite its high lethality, the Ebola virus survives little more than 30 seconds outside a bodily fluid, and infection rates are considerably lower than for other diseases.
The initial symptoms appear 2 to 21 days after infection and are similar to those of other viral infections – fever, weakness and joint pain. These are followed by vomiting, diarrhoea, impaired function of vital organs and, in some cases, internal and external bleeding.
In the more than a dozen outbreaks that have occurred in seven African countries since 1976, the disease has shown mortality rates ranging from 22% to 88%. In the current outbreak, the average case fatality rate was 50%, although lethality varied between patients and along the outbreak. According to recent studies, the mortality is directly associated to the level of circulating virus in the patient (viremia).
Drug Development
To date, there is still no approved drug to treat Ebola virus disease. However, early supportive care with certain basic interventions can definitely increase the patient’s probabilities of survival. These measures include rehydration with intravenous fluids and saline solutions, maintaining oxygen status and blood pressure, and treating other infections if they should occur.
For the first time, Ebola represented a real threat to the western world. This led to the unprecedented acceleration of clinical trials for a series of treatments and vaccines that had been developed for biosecurity reasons, but whose efficacy had never been tested.
Under the compassionate use principle, several promising drugs were tested. One of these, a cocktail of monoclonal antibodies against the viral glycoprotein (Zmapp, produced by Mapp Biopharmaceuticals) was used to treat several Ebola patients repatriated to western countries. Thanks to the collaboration between NGOs such as Doctors without Borders (MSF), scientists and international agencies, several clinical trials were initiated in order to test the efficacy of survivor blood plasma as well as antiviral therapies such as brincidofovir (produced by Chimerix, USA), favipiravir (developed by Fujifilm in Japan) and TKM (a viral RNA inhibitor developed by Tekmira in Canada).
However, due to a series of logistical and ethical issues (giving placebo to some of the patients is ethically questionable in the case of deadly diseases), the different clinical trials in the field started too late, when the number of patients had greatly decreased, and therefore did not yield conclusive results. The efficacy of the drugs developed during this outbreak may only be tested if scientifically and ethically sound clinical trials are designed and quickly implemented during the next outbreak.
Great progress was also made in terms of diagnosis, with several rapid detection tests developed and even validated in the field. These tests represent a crucial tool to stop viral transmission in health care settings, and their availability and affordability in the affected countries needs to be guaranteed.
The Most Promising Vaccines
An effective vaccine would be extremely useful to protect the health care professionals and scientists working in the field. It could also be used to protect the close contacts of a patient as well as the vulnerable populations who avoid health centres for fear of contagion.
Luckily, two Ebola vaccine candidates aready existed at the beginning of the outbreak, one based on the chimpanzee adenovirus (chAD) and the other based on the vesicular stomatitis virus (VSV), and were ready to be tested in clinical trials. Thanks to the collaboration between scientists, institutions and NGOs, these vaccines passed directly from phase I to phase III clinical trials. Despite these efforts, the trials started too late, when there were almost no patients left. The rVSV-EBOZ vaccine, tested in Guinea using a ring-vaccination strategy, gave preliminary efficacy results that were extremely promising. Although the efficacy of the chAD3-ZEBOV could not be tested, as study done with healthy African volunteers shows a good level of immunogenicity that, when combined with a boost immunization, could confer a long-lasting protection. Currently, the WHO is preparing the recommendations for the use of these vaccines in this and other outbreaks, and the Global Alliance for Vaccination and Immunization (GAVI) has signed a 5 million USD deal to guarantee the production and stockpiling of 300,000 vaccines for the next outbreak.
What We Still Don’t Know
This outbreak has clearly shown that many open questions remain concerning the virus, and that the problems are not necessarily over for those who overcome the disease. Recent studies show that the virus can persist up to 9 months after symptom onset in the semen of survivors, and that this can be source of new infections by sexual transmission. Some rare cases have also been reported where the virus gets reactivated after remaining dormant in immune-protected sites such as the eye and the central nervous system , although further research is needed to determine the frequency and the transmission risk of these events.
Thanks to the high number of survivors in this outbreak (17,000), it is becoming clear that, even if the virus is cleared, many survivors suffer from long-term health consequences such as chronic joint pain, visual and neurological disorders, and hair loss. Several ambitious projects (e.g. PREVAIL, a US-Liberia collaborative Project) have been launched with the objective of following-up the survivors to better understand the post-Ebola syndrome.
People who survive the disease develop natural immunity that can last for at least 10 years, although it is not clear whether immunity to one species of Ebola will protect against the other species. Interestingly, in this outbreak some people developed antibodies against the virus without ever getting sick. The frequency of this event remains to be determined, but it could imply that the case fatality rate for Ebola is actually lower than previously thought.
From the Disease to the Pandemic Threat…
Looking backwards, one could say there were two epidemics. In Western countries, where only three people were infected, it was an epidemic of panic caused, at least in part, by a deficient communication from the part of health authorities that in turn fed the media alarmism. In West Africa (mainly Guinea, Liberia and Sierra Leone), it was an epidemic that killed more than 11,000 people and generated chaos, immense suffering and fear that was further amplified by the lack of political leadership and international response.
Several experts have pointed out that, in spite of its virulence, the Ebola virus did not, in the past, warrant much attention from the international scientific community and funding agencies. After all, they argued, more people died in the poorest countries from malaria and tuberculosis on any given day in 2013, than those that died from Ebola, even in this outbreak. This attitude changed drastically, however, when the disease threatened to become a pandemic.
The fact that this has been the largest and longest Ebola epidemic recorded in history is not due to a more dangerous or infectious virus (in fact, the average mortality, of 50%, was lower than that of other outbreaks). It is rather the result of an infection that for the first time escaped the rural isolated areas and hit densely populated urban areas, where the person-to-person transmission became unstoppable. The factor that most contributed in shaping the crisis was the poverty and vulnerability of the communities living in the affected areas, where the fragile health systems were unable to curb the spread of the disease. All three most affected countries were at the bottom of the list in terms of healthcare. According to Afri-dev.info , before the crisis Liberia had 44 doctors, 1,131 nurses and 335 pharmacists for a total population of 4.2 million people. The situation was not much better in Sierra Leone or Guinea, with 2 and 10 doctors for each 100,000 inhabitants, respectively, compared to Spain, for example, that has 370. After the crisis, the situation is even worse: more than 500 health care workers have died from Ebola in the three countries.
Another factor that hampered the resolution of the crisis was the slow and uncoordinated response at the national (none of the three countries had previous experience with the Ebola virus) and the international level. Already in mid-March of 2014, Doctors without Borders described the international response as “non-existent”. It wasn’t until August 8 of 2014, when the epidemic was already out of control, that the WHO declared the situation as a public health emergency of international concern.
Finally, the third factor that further amplified the epidemic was the lack of rapid and reliable diagnostic tools, as well as the absence of efficient preventive and therapeutic treatments. However, some studies show that, at the peak of the crisis, control and prevention measures such as the identification and isolation of suspected cases and proceeding with safe burials were as or more efficient in curbing the disease than a ring vaccination strategy would have been. The implementation of such control and prevention measures was possible only after the establishment of an efficient dialogue with the community to ensure its engagement, and became one of the major lessons from this epidemic.
…and from the Epidemic to the Control
Thus, after two years of great efforts to implement the measures to ensure surveillance, case identification and community engagement, the number of new weekly cases decreased to less than 10 over the last five months of 2015, and on January 14 the WHO declared the whole region free of Ebola virus transmission. However, a case reported in Sierra Leone a few hours after the announcement highlighted the risk of disease re-emergence due to viral persistence in some survivors, as well as the need to maintain a heightened surveillance system.
It has become clear that the Ebola virus will remain in the region, hidden within animal reservoirs and some survivors, and will continue to cause new outbreaks of considerable impact in the absence of additional control tools and strategies.
The Three Ebola Crises
The epidemic’s consequences are devastating. More than 11,300 people have died in two years, a tragedy whose repercussions go well beyond the direct death toll. In a continent where malaria alone takes half a million lives, the impact of Ebola on the health systems and the social and economic stability of the region suggests that the crisis is far from over.
The Direct Victims
By ends of January 2016, roughly 28,000 people were infected in Guinea, Liberia and Sierra Leone, of which 11,300 died. In addition, there were isolated cases in other countries of the region that managed an efficient control of the outbreak (like Nigeria, Senegal and Mali) and even in more distant countries where the disease arrived with imported cases (two infections in USA and 1 in Spain) .
Health Consequences
Although in 2012 malaria was responsible for 7,000 deaths in Sierra Leone, Liberia and Guinea, the efforts to remedy this and other high-risk situations had begun to bear fruit in recent years during the post-conflict transition period. Around 60% of children under five were receiving antimalarial treatment. At least one in every two women gave birth with the assistance of skilled health care personnel (data from WHO African Health Observatory ) and the average public expenditure per patient had increased significantly in all three countries (threefold in Guinea and fivefold in Liberia over the last decade)
All this progress has partly gone down the drain as a result of Ebola. The epidemic scared patients (women and children in particular) away from healthcare facilities and drastically reduced the possibilities of the system to meet the needs of other diseases and continue with vaccination campaigns. More than 500 medical doctors, nurses and midwives died from Ebola in the three countries.
Several studies have tried to quantify the number of indirect deaths caused by the epidemic. One study estimates an additional 11,000 deaths from malaria, HIV and tuberculosis in the three countries, for 2014. Only in Guinea, it is estimated that 74,000 cases of malaria went untreated in 2014, and that the number of children treated for diarrhea and acute respiratory infections decreased in 60% during the same period. Another study calculated an increase in maternal mortality ranging from 38% in Guinea to 111% in Liberia. UNICEF estimates that 70,000 births in Liberia have not been registered since the outbreak began. Finally, several experts have warned of the danger of neglecting the basic health systems and child survival interventions in these countries as a result of centering all efforts and resources on the Ebola response.
Socio-economic Consequences
Ebola has also wiped out much of the progress achieved through considerable political, social and financial efforts by local and international authorities after the wars that devastated the region, and has destroyed hopes of economic improvement in the coming years. Initially, it was considered a sanitary crisis rather than a humanitarian one, and the long-term consequences on education, livelihood and political stability were neglected. The World Bank estimates (updated in April 2015) that the three countries will lose at least US$2.2 billion in forgone economic growth in 2015 as a result of the epidemic. In Sierra Leone, where the mining activity basically came to a halt, the economy will shrink by 23.5%. In Guinea, the mining activity was less affected but nevertheless economic gwoth will fall from to 4.3% to -0.2% and only Liberia will continue growing although at a rhythm of 3% instead of 7%. For each Ebola death there is a productivity loss that ranges between 11,238 international dollars for Liberia and 47,364 for Nigeria, according to a study.
The cost of recovery will far outstrip the total amount of aid received by the three countries in the past, and is calculated to be of US$812 million for Liberia, US$844 million for Sierra Leone and US$2,890 million for Guinea for the 2015 to 2017 period.
In terms of food insecurity, the World Food Program provided an early estimate whereby at least 3.6 million people were at risk of being food insecure during 2015.
Finally, the social consequences are many and include the proloned closure of schools and the consequent increase in teenager pregnancies, the large number of orphans (16,000 children that lost one or both parents, according to UNICEF), and the stigmatization of survivors, healthcare workers and safe burial team members.
The Two Sides of the Response
The international community’s response has been largely criticized and with reason. However, the response has also revealed another face.
The Worse
Despite repeated warnings by Doctors without Borders since March 2014, the international response did not kick-in until the situation was completely out of control. Foreign aid (both human and financial) started to arrive in September 2014, when the United Nations created UNMEER, its first health-specific mission. Even then, the organizations working in the field struggled to translate the arriving resources into efficient actions, according to a report by Save the Children.
The initial response was also hampered by other local issues, such as the lack of communication, community participation and trust in authorities. Instead of working together with the communities to find how to best protect the people, reduce the fear and ensure safe burials, the initial response worked without or even against them. The response was also complicated by the clash of individual rights versus the interest of the society or the country.
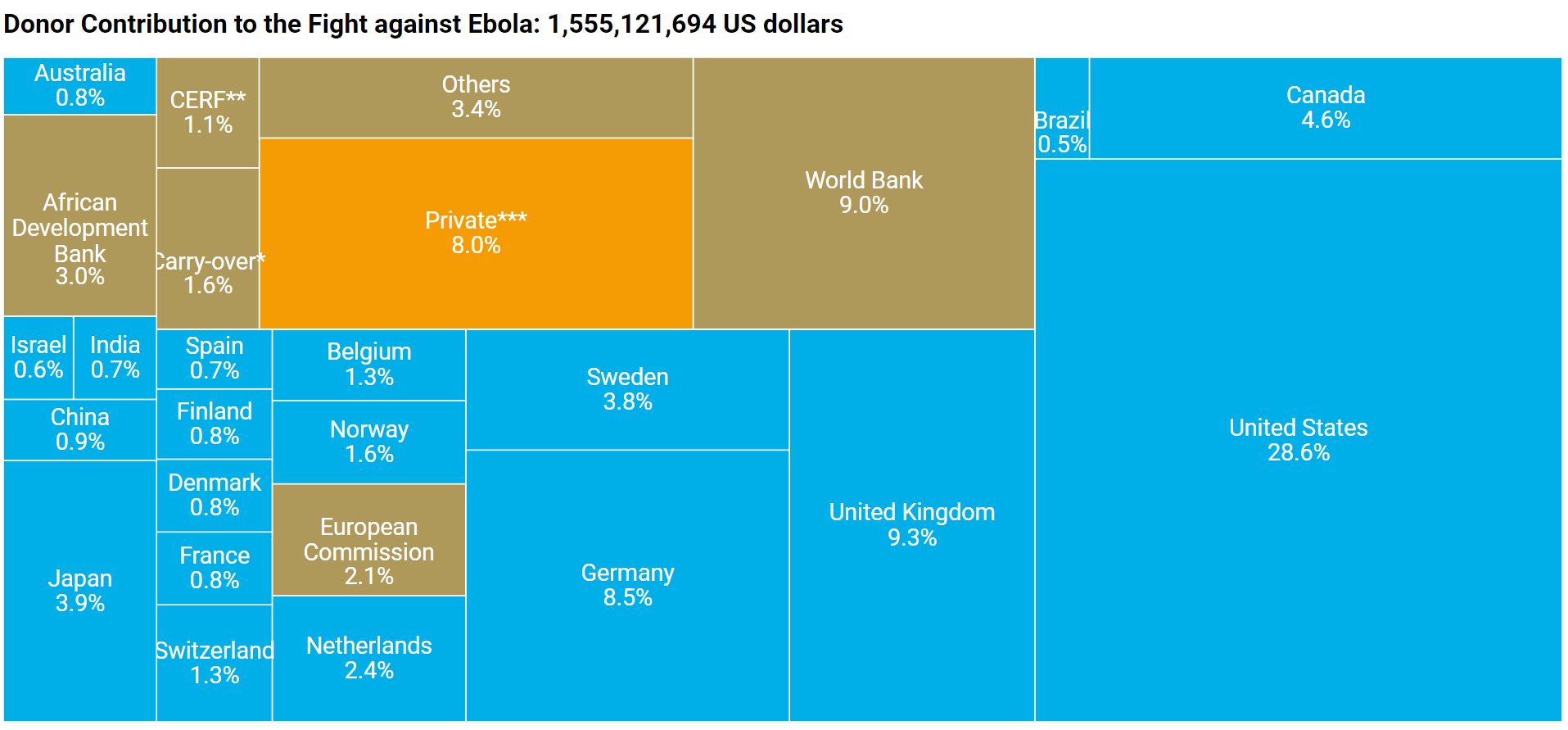
The necessary resources, estimated at 15 million in April 2014, grew to US$1,500 million in December 2014 (according to OCHA). By January 2015, the different donors (governments, multilateral organizations, NGOs, private sector) had committed to give the impressive amount of US$3,500 million although in July 2015 more than 600 million were still not paid.
The Best
Notwithstanding, it is only fair to point out that 2013 was a year marked by worldwide crisis, during which the total mobilized resources reached the record amount of 22,000 million USD. The WHO was struggling with the MERS outbreaks in Saudi Arabia and the polio reapprearance in Syria.
The achievements at the national and international level also deserve to be acknowledged. More than 40 0rganizations and 58 foreign medical teams (2,500 people) were deployed in more than 60 specialized treatment centres. The international response included medical teams from China, Cuba, the African Union, the UK and USA. Only in Liberia, the Mercy Corps received support from 76 organizations and coordinated more than 800 healthcare workers to train more than 1,500 community workers that in turn provided crucial information on protective measures to more than 2 million Liberians.
The European Union, also criticized for its late and uncoordinated response, has contributed (to date of July 2015) with 1,800 million euros, including funds from Member States and almost 900 million from the European Commission. One of the main contributions by the EU was the establishment of mobile laboratories in the three countries to facilitate patient screening and training of personnel (EMLab and EIWAM-Lab projects).
At the end of the crisis, the NGOs have been strengthened by their key role, not only in humanitarian aid but also in collaborating with scientific institutions and agencies in the development of research projects and clinical trials.
Hence, as the Overseas Development Institute (ODI) concludes, the Ebola crisis brought out the best (dedication, diversity and resourcefulness) and the worse (unpreparedness, dependence on donors, confrontation with the socio-cultural context) of the international response. The key to success lies in understanding the relations of relationships of power and culture in the communities where the outbreaks occur in order to treat the causes and not only the symptoms of the problem.
Lessons for Global Health
The Ebola crisis offers a number of instructive lessons that are also relevant to other major global health challenges.
Development as a matter of mutual interest: Reducing the health equity gaps between countries is an exercise in self-interest as well as an ethical obligation. The Ebola crisis demonstrates the extent to which our interests overlap with a global health system. The origin of the Ebola epidemic lies in the inability of the national public authorities and the donor nations to adequately strengthen the health and education sytems in West African countries. We can find similar examples in other areas that are a priority for Europe’s interests, such as the security crisis in the Sahel and the migratory pressure on Europe’s southern borders.
The dysfunctional system governing pharmaceutical innovation and access to medicines: The delay in the development of preventive and curative treatments for Ebola poses fundamental questions on how equitable our current R&D system is and how effective are the current research incentives. The development of an Ebola vaccine was only been speeded up in recent months, following a period of neglect that began in the 1980s and ended only when it started to appear likely that a preventive treatment would be useful for wealthy countries or profitable for private pharmaceutical companies. Francis Collins, director of the US National Institutes of Health (NIH), stated at the time that a vaccine would already be available had it not been for the budget cuts that have affected public research over the last decade. ISGlobal has first-hand experience with the failures of drug markets in other areas such as malaria, Chagas Disease and antibiotic resistance.
The role of development cooperation: The response to the Ebola crisis became an arena for the new international diplomacy. Small economies like Cuba and Denmark have joined forces with African countries and larger powers, such as the USA and the UK, in an exercise of shared responsibility through development aid. In the 21 st century, cooperation is a major tool for countries to exercise global influence, resolve their own problems, and building the image they want to project.
The Cost of Inaction
The Ebola crisis has shown that, in global health, turning a blind eye may result much more expensive than acting on time. Spain is one of the countries that paid a high price because of the international community’s inability to curb the epidemic. Since the first medical missionary was repatriated in August 2014, Spain treated three confirmed cases (two of them fatal) and a dozen patients were monitored for suspected disease.
The total cost of these operations was never revealed by the Spanish government, but an estimate made by ISGlobal on the basis of information provided by the authorities and consultation with health management experts, suggests that Spain may have spent more than 17 million euros, which amounts to almost 6 million per infected patient treated in our country. Importantly, the amount spent in fighting the disease in Spain is twice the amount that the government allocated to fighting it in West Africa.
10 Essential Reforms
The international community has learnt a bitter lesson as a result of the Ebola crisis in West Africa. The WHO has recognized its responsibility and has mandated a series of reforms and the creation of global health emergency workforce to guarantee its rapid response to outbreaks and emergencies worldwide. The crisis has also highlighted the urgent need for national and international investment in the affected countries in order to strengthen the health and surveillance systems, as one of the major priorities.
A panel of experts from Harvard University and the London School of Tropical Medicine and Hygiene, have proposed 10 essential reforms in order to avoid similar tragedies in the future.
Blog Posts about Ebola
The Three Crises of Ebola is a publication by the ISGlobal Policy team: Laia Bertran, Gonzalo Fanjul, Adriana Orbea, Pau Rubio, Adelaida Sarukhan y Elena Villanueva. Graphic design: Anna Barberà. Visualizations: Data'n'Press. Coding: Óscar Rodríguez/Sonicon.