A majority of Malaria Infections in Children in Papua New Guinea are Due to the Reactivation of Dormant Liver Stages of Plasmodium vivax
Mass administration of drugs that target both blood and liver parasites represents a highly effective strategy for preventing relapsing infections and reducing disease transmission
03.11.2015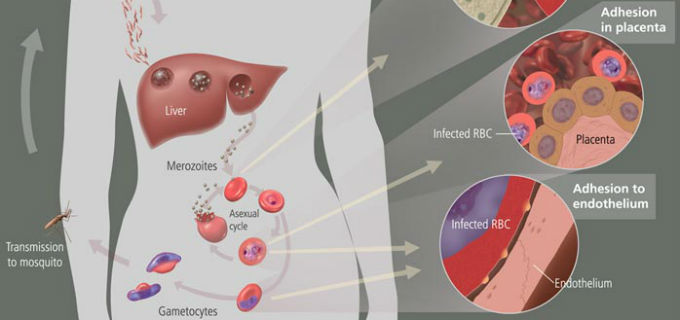
A large clinical trial led by Dr. Ivo Mueller, researcher at ISGlobal and the Walter and Eliza Hall Institute, Australia, shows that a great majority of P. vivax infections among children in Papua New Guinea are caused by the reactivation of hypnozoites, a dormant liver-stage of the parasite, and that these relapses contribute importantly to sustaining disease transmission. Further results of the study, published in Plos Medicine, indicate that massive drug administration campaigns combining blood- and liver- stage treatments are highly efficient for reducing P. vivax transmission and thereby provide important evidence-based recommendations for policy makers.
Over the last 20 years, there has been a significant reduction in overall malaria incidence. In parallel, outside Africa there has been a shift in Plasmodium species, with P. vivax now accounting for more than 90% of clinical cases in the vast majority of countries. P. vivax has the ability to relapse weeks, months or years after primary infection, due to the reactivation of dormant stages in the liver. These stages cannot be detected by current diagnostic tools and are not targeted by commonly used anti-malarial drugs unless a 7-14 day administration of primaquine is added to the treatment.
The authors wished to determine the contribution of P. vivax relapses to disease in children in malaria-endemic areas of Papua New Guinea, where all four human Plasmodium species co-exist. For this, they conducted a primaquine mass-treatment study in PNG children aged 5 to 10 years where all infections were diagnosed with a sensitive molecular test, and used the data in a mathematical model to predict the efficiency of massive drug administration (MDA) as compared to mass screening and treatment (MSAT) approaches.
For Dr. Mueller, the study has two important outcomes. First, the clinical trial shows that a great majority of infections by P. vivax in the region are caused by relapsing infections because the drugs directed against the blood-stage of the parasite do not have activity against the liver parasites. The second component is its relevance for public health policies. MSAT (screening everyone and treating only those that are positive) against the non-relapsing P. falciparum only works if the diagnosis test is good and less expensive than the treatment itself, which is currently not the case. For P. vivax it will not be effective because it does not detect and remove the dormant liver infections. The study however predicts that MDA (treating everyone) may work better and be more cost-effective, killing a larger percentage of parasites within the population, if drugs against the liver stage are included. "The problem", explains Dr. Mueller, "is that these drugs can be toxic to people that are deficient for an enzyme, although there is a test to identify such people".
He concludes that better epidemiology studies (to identify risk groups susceptible to benefit from focal MDA) together with better diagnostic tools (for example serological screens that are sensitive enough to detect liver-stage parasites) are urgently needed to reinforce malaria elimination efforts.
Reference:
Robinson LJ, Wampfler R, Betuela I, Karl S, White MT, et al. Strategies for Understanding and Reducing the Plasmodium vivax and Plasmodium ovale Hypnozoite Reservoir in Papua New Guinean Children: A Randomised Placebo-Controlled Trial and Mathematical Model. PLoS Med. 2015 Oct 27;12(10):e1001891.



