Interview with Myron Levine: "The Anti-Vaccine Movement is One of the Biggest Problems We Face"
The leading expert talks about challenges and opportunities in the vaccine field
30.03.2015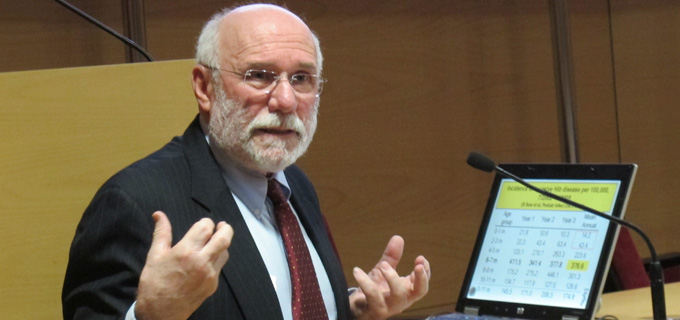
Myron Levine has a longstanding experience in vaccinology: he participated in the smallpox eradication campaign, formed part of the first work group of the Global Alliance for Vaccination (known as GAVI) and funded the Centre for Vaccine Development (CVD) in Maryland, which he still directs. Since August 2014 he has been in the frontline collaborating with WHO in the development of an Ebola vaccine. He answered some questions regarding opportunities and challenges in the field of vaccinology.
Which is the most difficult challenge in the vaccine field?
I think that for most vaccines against most pathogens, the science is pretty easy. There are a few exceptions, for example malaria, HIV, TB, but for many pathogens making a scientifically plausible vaccine that could go all the way to licensure and become a public health tool, if the funding is available, is actually pretty easy. The next really big hurdle is the financing to get that vaccine to the developing world. At the end of last century the birth of GAVI took place within the UN system. The global alliance for vaccines and immunization was so successful that its nickname came to be its new name- the GAVI alliance. It has a lot of capital funding that has succeeded in introducing multiple new life-saving vaccines and has strengthened immunization services in the developing world, but there are more candidates that are seeking GAVI funding than GAVI can possibly fund. So one problem has been solved and new problems emerge because of this. But this is progress.
The single biggest problem at the global level that I see is what we call vaccine hesitancy and anti-vaccine lobbying. So there are people who, almost like a religion, are against vaccines. If you read their websites, they are put together brilliantly: they take a quote here, a sentence from a paper, they put it all together as a patchwork quilt in a logical way and they create a convincing argument on why you should not take a vaccine. They create a smoke and they foster hesitancy. Take a young set of affluent, well-educated parents with a new baby: they see the smoke and think there must be some fire, there must be some truth. When a vaccine gets rid of a disease, like going from hundreds of thousands of cases of measles to almost none, parents wonder whether it's appropriate to give their child the vaccine, forgetting that it's the high coverage of the vaccine that made the disease disappear. We are seeing the appearance of this vaccine hesitancy in Latin America for example, even in places that were strongly pro-vaccine two generations ago. I see this also appearing in sub-populations of some of the poorest countries; because of internet we have a so-called flat world.
I see the anti-vaccine movement as one of the biggest challenges and problems lurking out there. We can never prevent measles mortality in sub-Saharan Africa in a cost-effective way and we can't do elimination when we still have measles in Switzerland, Japan or France.
Do you see any major obstacle for the Ebola vaccine?
Clearly we need to have potent vaccines. But we also need to think strategically, using good epidemiologic planning, on how we use the vaccine. Even a vaccine that only gives short-lived protection can still be a public health tool to interrupt transmission if we use it in the right way.
The current Ebola crisis has proved that the process for vaccine and drug testing can be greatly speeded. In your opinion how can the drug development system improve without compromising safety?
That's a great question. I think we live in a world where it's a matter of balances. So if you have a vaccine against a disease that's very common, that causes some morbidity, that is not a killer infection but can interrupt the economy and therefore there is a desire for the vaccine, it will not get licensed unless it has a very high level of safety and its adverse reactions are uncommon and mild. Whereas if you have this once in a lifetime situation as we see with Ebola, that breaks all the rules: to go from phase I to phase III without phase II results; to go from a vaccine that had never been in a human being to a dose selected six months later; this is unheard of! This only occurs in an epidemiological situation. Actually, it was more than that, it was a phenomenon. We get two newspapers at home and Ebola was on the front page day after day. It was amazing.
One in five children is unprotected against vaccine-preventable diseases. Why do you think that inequalities in vaccination still exist?
I think we need to separate the first world from the developing world. In the first world it is because we got rid of the infections, in part thanks to vaccines, that people are willing to play the lottery. Measles is the example. These parents that make the choice with measles do not recognize that even in modern Europe and USA about 1 in 600 individuals who contract measles will die and there will be hospitalizations.
In the developing world it's more about access to health care and having funding from GAVI or otherwise to provide the vaccines. It's having a proper infrastructure to keep the cold chain. The measles vaccine is notorious for having a very limited duration of potency in a hot tropical environment.
So it's a different set of challenges and I think the latter ones are easier to solve than the first ones. We are grappling right now with legislation in the USA, where each state decides whether parents may ask for an exemption. The problem with exemptions on the basis of religious or intellectual decisions is that children who may have illnesses that do not allow them to be vaccinated depend on other children being vaccinated to stay alive. Many of us see that as unfair. I would love to see a very compulsory, no exceptions legislation for some infectious diseases.
Can you tell us what new vaccines will be available soon?
There are a lot of exciting developments. There has just been a new meningitis vaccine and a second polyvalent vaccine. There's a new concept that is really gaining popularity, which is immunizing pregnant women in the third trimester to prevent infectious diseases in the infants who are too young to get vaccine coverage. There is currently a consortium of three independent field trials with influenza vaccine to answer this question: Can immunizing the mother protect the infant less than 6 months of age against influenza? We carried out one of those trials in Mali and we can categorically answer that in Mali, the least developed of the three countries (the others were South Africa and Bangladesh), it really does work. That's now taking off and we're looking at preventing pertussis. I see this as one of the areas that is going forth.
In the developing world we are also looking at Shigella vaccines that are starting to move to field trials. There is a new generation of typhoid vaccines called Vi conjugate, where a polysaccharide is linked to a carrier protein to change its properties. One conjugate was licensed last year in India and looks very attractive. A lot is going on. Those are just a few examples.